
.%20at%2012%20yrs.jpg)
Patients with open fractures and/or vascular injury were excluded. The purpose of this study was to evaluate the outcomes and complications of Gartland type III pediatric supracondylar humerus fractures treated at a pediatric level-one trauma center over a 7-year period, specifically addressing the impact of the time to surgery on the incidence of postoperative complications and conversion to an open reduction.Īll children with closed type III supracondylar humerus fractures admitted and treated between January 2004 and December 2011 at the author’s institution were identified. With regards to operative delay leading to open reduction, there is literature supporting both arguments, resulting in a lack of conclusive agreement. showed that delayed intervention resulted in an increase in open reduction but no other perioperative complications. Multiple studies followed showing similar results. published a retrospective review comparing early versus delayed (greater than 8 h following fracture) treatment of 58 patients with type III fractures and showed no difference in terms of clinical results or perioperative complications, including conversion to open reduction. In a similar fashion, many pediatric studies have been performed questioning the necessity of urgent night-time intervention in Gartland type III supracondylar humerus fractures. In recent years, many adult trauma hospitals have decreased night-time on-call orthopedic surgery without affecting patient outcomes by allowing dedicated trauma operative time during the day. The theoretical advantage proposed that this would lead to a decrease in perioperative complications, including iatrogenic nerve palsies, compartment syndrome, and conversion to an open reduction. Until the late 1990s, it was believed that displaced pediatric supracondylar humerus fractures required emergent surgical intervention or skeletal traction. conducted a systematic review focusing on iatrogenic ulnar nerve injury due to the placement of a medial pin and concluded that the number needed to harm was 28 patients. The concern for iatrogenic ulnar nerve injury during the placement of a medial pin discourages this configuration. Biomechanical testing has demonstrated a theoretical advantage of both medial and lateral cross pinning however, these initial findings have not translated into clinical results.
The focus of many recent research studies on the treatment of these fractures has been pin configuration. The current preferred treatment for Gartland type III fractures consists of attempted closed reduction and percutaneous pinning.

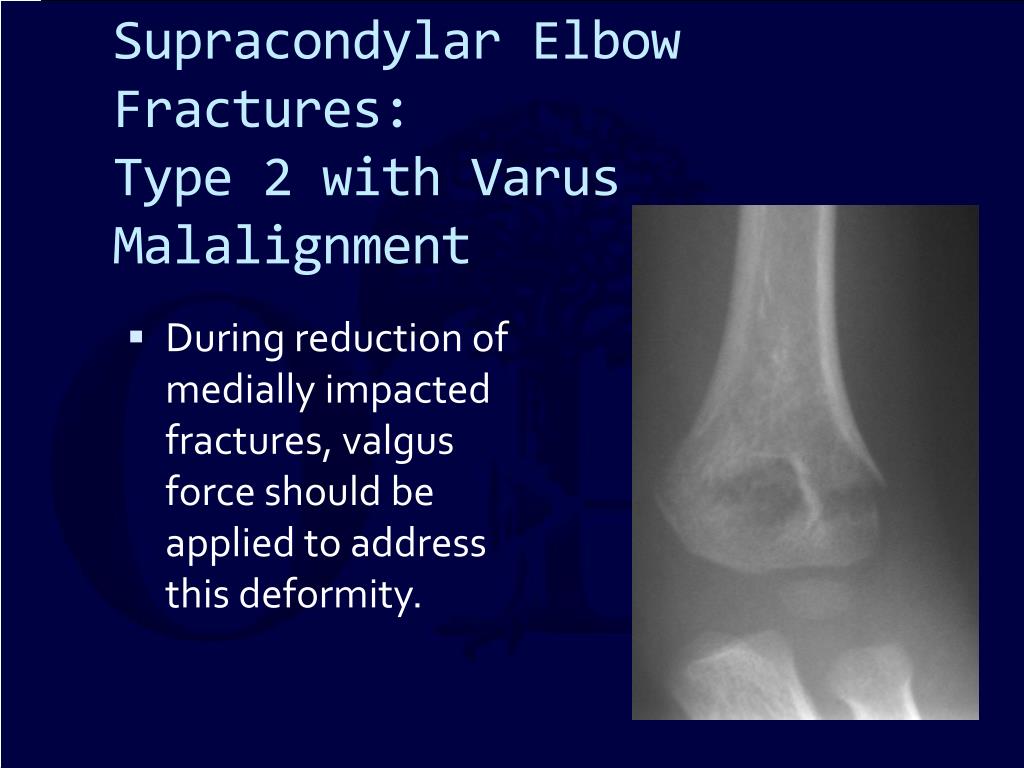
Gartland originally described a classification for extension-type supracondylar humerus fractures, dividing them into three types: type I is non-displaced, type II is displaced with an intact posterior cortex, and type III is displaced without cortical contact. The majority of these fractures (96–98 %) are extension-type fractures. Provider unable to clinically determine whether the condition was present at the time of inpatient admission.Supracondylar fractures of the humerus are the most common fracture of the elbow in children. POA Indicators on CMS form 4010A are as follows: Indicatorĭiagnosis was present at time of inpatient admissionĭiagnosis was not present at time of inpatient admissionĭocumentation insufficient to determine if the condition was present at the time of inpatient admission.Ĭlinically undetermined. A 'billable code' is detailed enough to be used to specify a medical diagnosis. S72.462D is a billable ICD code used to specify a diagnosis of displaced supracondylar fracture with intracondylar extension of lower end of left femur, subsequent encounter for closed fracture with routine healing. This "Present On Admission" (POA) indicator is recorded on CMS form 4010A. POA Exempt Code The Center for Medicare & Medicaid Services (CMS) requires medical coders to indicate whether or not a condition was present at the time of admission, in order to properly assign MS-DRG codes.


 0 kommentar(er)
0 kommentar(er)
